Posted by Dr Farah Arshad | Breast Cancer doctor in Lucknow
When doctors say “triple negative breast cancer,” most people hear the word aggressive and feel scared. But what does it actually mean? Why does it behave differently? And what can you do about it?
Let me break it down in the simplest way possible.
What Does “Triple Negative” Actually Mean?
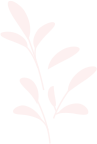
Breast cancer cells usually feed on hormones like estrogen or progesterone, or a protein called HER2. Doctors use these to target the cancer with specific medicines.
Triple negative means the cancer tests negative for all three of these. So the usual targeted treatments do not work. This is why it is harder to treat — not because it is impossible, but because fewer weapons are available.
Why Is TNBC Called Aggressive?
Here are the main reasons, explained simply:
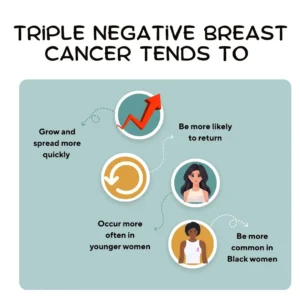
It grows fast. TNBC cells divide quickly. The faster cancer grows, the more chances it has to spread before it is caught.
It spreads early. Even at an early stage, tiny cancer cells can travel to other parts of the body through the blood. This is called micrometastasis, and it happens silently.
It mutates quickly. Because TNBC often has faulty DNA repair, the cancer keeps changing. Some cells become resistant to chemotherapy. When chemo kills the sensitive cells, the resistant ones grow in their place.
It lacks easy targets. With hormone-positive breast cancer, doctors can use hormone-blocking pills for years. With TNBC, there is no such option. Chemotherapy is the backbone of treatment.
TNBC Is Not One Disease — It Is Several
This is something most people are not told. “Triple negative” is just a label that means three tests came back negative. Inside that group, there are actually many different types of TNBC:
| Type of TNBC | Key Feature |
|---|---|
| Basal-like | Most common subtype, often fast-growing |
| Immune-rich | More likely to respond to immunotherapy |
| Immune-cold | Less responsive to immunotherapy |
| BRCA-associated | Linked to inherited gene mutation, may respond to PARP inhibitors |
| Androgen receptor-positive | May respond to anti-androgen therapy |
| Mesenchymal-like | More prone to spreading |
This is why two patients with the same stage of TNBC can have very different outcomes. The subtype matters just as much as the stage.
When Does TNBC Come Back?
This is one of the most important things to understand. TNBC follows a very specific relapse pattern:
Risk is highest in the first 3 to 5 years. If cancer comes back, it usually does so within this window.
After 5 years, the risk drops significantly. This is actually good news. If a patient reaches the 5-year mark without recurrence, the long-term outlook improves a great deal.
This is different from hormone-positive breast cancer, where the risk of recurrence can stretch across 10 to 20 years.
Where Does TNBC Spread?
TNBC tends to spread to specific organs more than others:
| Common Spread Sites in TNBC | Less Common in TNBC |
|---|---|
| Lungs | Bones |
| Brain | Liver (less dominant) |
| Distant lymph nodes |
Hormone-positive breast cancer more commonly spreads to bones. TNBC more commonly goes to the lungs and brain. This changes what symptoms to watch for and what scans to prioritize.
BRCA and TNBC — What Is the Real Connection?
Yes, TNBC is more common in people who carry a BRCA1 gene mutation. But this is often misunderstood. The truth is:
Many TNBC patients do NOT carry a BRCA mutation. And not everyone with a BRCA mutation develops TNBC. Genetic testing and counseling helps figure out which category a patient belongs to, because treatment decisions — especially around PARP inhibitors — depend on this.
What Is Neoadjuvant Chemotherapy and Why Does It Matter?
In TNBC, chemotherapy is often given before surgery. This is called neoadjuvant chemotherapy. It has two big purposes. First, it shrinks the tumor so surgery is easier. Second, it works like a test. If the cancer completely disappears before surgery, that is called a pathologic complete response, or pCR. Patients who achieve pCR generally have much better long-term outcomes.
If cancer cells remain after chemotherapy, it means those cells were resistant. This changes the plan. Doctors may escalate treatment or add different medicines to address the remaining disease.
What About Treatment Side Effects?
TNBC treatment is intensive. It often involves multiple types of chemotherapy drugs and sometimes immunotherapy. Side effects that patients should be aware of include heart-related changes from certain chemotherapy drugs, nerve damage in the hands and feet, early menopause in younger women, and memory or concentration changes sometimes called chemo brain.
These are real, and they affect quality of life. Talking to your doctor about managing these side effects is just as important as the cancer treatment itself.
5 Frequently Asked Questions About TNBC
1. Is triple negative breast cancer always fatal?
No. Many patients with TNBC — including those at advanced stages — achieve remission and go on to live full lives. Outcomes depend on the stage at diagnosis, the specific subtype, response to treatment, and overall health. Early detection and completing treatment as planned significantly improve survival.
2. Does TNBC run in families?
It can, especially when linked to BRCA1 mutations. However, many TNBC cases occur without any family history or gene mutation. If you are diagnosed, genetic counseling is recommended to understand your personal risk and implications for family members.
3. Can TNBC be treated without chemotherapy?
Currently, chemotherapy is the main treatment for TNBC. However, immunotherapy has shown significant benefit in certain subtypes, especially immune-rich tumors. Research into newer targeted therapies is ongoing, and options are expanding.
4. Is TNBC more common in younger women?
Yes. TNBC is diagnosed more often in women under 40 compared to other breast cancer types. It is also more common in women of African descent. This is why young women should not ignore new breast lumps or changes, even if they feel they are “too young” for cancer.
5. What happens if TNBC comes back after treatment?
Recurrence is most likely in the first three to five years. If it comes back as a local recurrence (in the same area), options still exist for treatment. If it comes back as metastatic disease, the focus shifts to controlling the cancer and maintaining quality of life. Each case is different, and treatment decisions are made based on where the cancer has spread and what prior treatments were used.
When Should You See a Breast Surgeon?
Do not wait if you notice any of the following. A lump or thickening in the breast or underarm. Skin changes such as dimpling, redness, or an orange-peel texture. Nipple discharge that is not related to breastfeeding. Any breast change that feels new or unusual.
TNBC often presents as a fast-growing lump. Early evaluation can make a meaningful difference.
Talk to Dr. Farah Arshad — Breast Surgeon in Lucknow
If you or someone in your family has been diagnosed with triple-negative breast cancer, or if you have concerns about a breast lump or family history of breast cancer, do not navigate this alone.
Dr. Farah Arshad is a specialist breast surgeon based in Lucknow with experience in the diagnosis, treatment, and surgical management of all types of breast cancer, including triple negative breast cancer.
She believes that every patient deserves a clear explanation of their diagnosis, honest answers to their questions, and a treatment plan that fits their individual situation — not a one-size-fits-all approach.
Book a consultation with Dr. Farah Arshad today. Early evaluation, the right diagnosis, and expert guidance can change your outcome. You do not have to figure this out alone.